[ad_1]
It started with one magical model, no dedicated space and a few staff who saw the transformative power of molded plastics, printed layer by layer into a physical, life-size anatomical representation.
This 3D-printed replica of conjoined twins was the big bang from which Mayo Clinic’s 3D anatomical modeling practice has exploded.
“We started doing 3D printing about 17 years ago at Mayo Clinic for a complex case involving congenital twins. And it’s expanded over that time frame to encompass every surgical subspecialty,” says Jonathan Morris, M.D., medical director and co-founder of the 3D Anatomic Modeling Unit at Mayo Clinic in Rochester, Minnesota. “The reason it started all in-house is because we have subspecialty expertise in each part of the process. We had these complex problems, and we found that 3D printing aided in understanding them in a three-dimensional, life-size way that 2D images could not.”
Growth and development
Over 17 years and counting, the practice has expanded in size and scope, with increasing square-footage dedicated at Mayo Clinic to the 3D Anatomic Modeling Unit in Rochester and new and growing spaces in Arizona and Florida.
Each group is led by dedicated physicians, researchers, engineers, technologists and more, all committed to ensuring these valuable tools are available to any physician, surgeon, researcher or educator who needs them. In addition to Dr. Morris, Rahmi Oklu, M.D., Ph.D., is medical director of the Arizona group. Elizabeth M. Johnson, M.D., is medical director of the Florida team, and Robert Pooley, Ph.D., is the technical director in Florida.
The space in the Joseph Building at Mayo Clinic Hospital – Rochester, Saint Marys Campus is now about 8,000 square feet of manufacturing space with 16 staff and 15 3D printers that use a broader array of materials than were available in 2006. The 3D Anatomic Modeling team in Arizona has about 1,000 square feet, nine printers and two staff, and the team in Florida has nearly 1,000 square feet, with additional space to allow for further expansion to almost 1,200 square feet, 10 printers and two full-time staff and five additional team members.
This growth ensures Mayo is able to meet the needs of the patient, Dr. Morris says. “The space and the technology we have are unique for a healthcare institution, but it only exists because the needs of the patients dictated it.”
At Mayo Clinic in Arizona and Florida, the lab spaces are newer endeavors than in Rochester, reflecting the surging demand for patient-specific models and cutting guides for individualized care — and for advancing the science. Arizona and Florida had 3D printers, but they now have homes to allow for continued growth.
“It’s nice. It’s brand-new, there’s a lot of orange — I like orange,” Dr. Oklu says of the new space in Arizona, which opened in 2020.
Where it started
In Rochester, the 3D Anatomic Modeling Unit finished construction in 2021 on an expanded space that better accommodates what has become a booming practice — with about 900 models and 1,200 cutting guides produced each year.
“Mayo Clinic is really setting the path for others to follow,” says Adam Wentworth, a senior engineer in the Rochester 3D Anatomic Modeling Unit. “The development of this space could not have occurred without the vision from administration and the passion of the leadership of Dr. Jonathan Morris and Dr. Jane Matsumoto, who started the lab. The effort that they have put in outside of their normal working hours to lift up the lab and communicate its capabilities to everyone else and the surgical champions who have communicated the benefit of anatomic modeling were also a huge factor in the success of the lab.”
He says the returns on the investments are apparent every day.
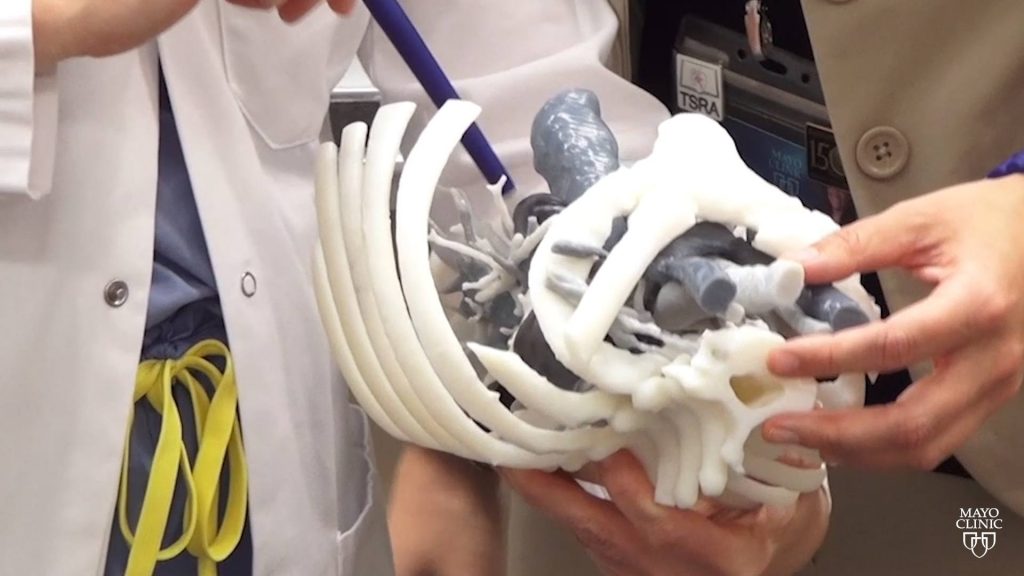
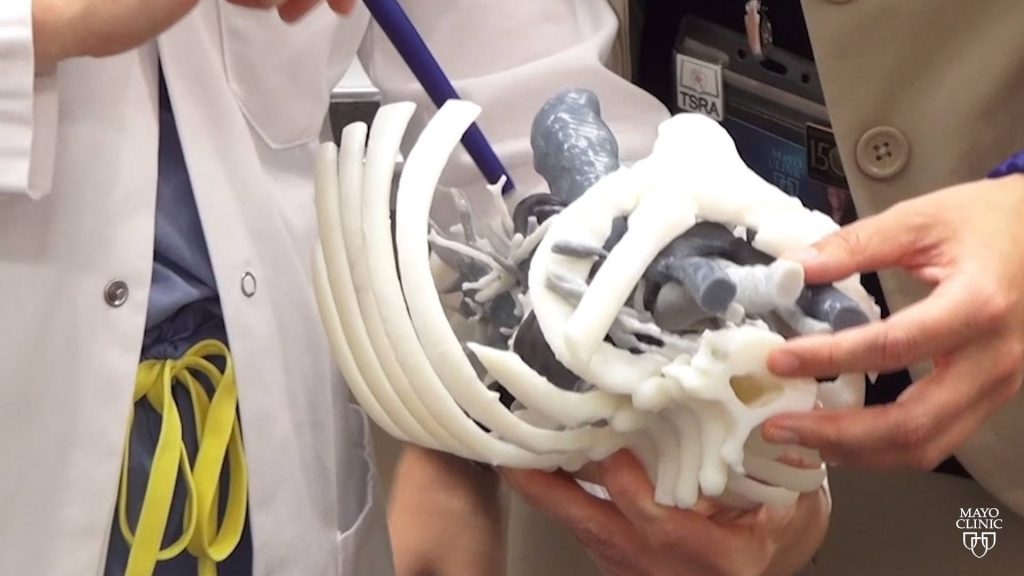
“Physicians and surgeons are able to have the life-size 3D model in their hands,” says Tori Sears, another engineer in the Rochester 3D Anatomic Modeling Unit. “They can visualize where a tumor is exactly located within the anatomy that’s usually covered up by soft tissue. They make measurements right on the model and can better understand through haptic perception where that tumor is located, what adjacent critical structures are nearby and what is the best approach to minimize procedure times.”
Dr. Morris says it is important to have the 3D anatomic modeling practice as part of the Department of Radiology.
“When you combine everything together and you centralize it within the Department of Radiology, you can serve just not one specialty, you can serve all of them,” he says. “We’re an integrated team of people who are coming together to solve complex surgical problems. And we’re using engineering, 3D printing, custom medical device manufacturing and surgical expertise all together, instead of each one of us working apart.”

Where it’s going: Arizona
Dr. Oklu says 3D printing in Arizona is a “three shields” endeavor, touching education, research and the clinical practice.
With the debut of the new space, Dr. Oklu had intended to provide opportunities for staff to learn about 3D printing — how the printers work and how to order models and guides. After being sidelined by the pandemic, that effort is restarting.
“My plan is to go to every department to present what we do and what we could do,” Dr. Oklu says. “I want to open it up so people can learn what 3D printing is. Everyone’s curious, they just don’t know how to do it.”
He says the lab won’t stray from what Florida and Rochester do on the clinical side. “I try to help, whatever the request is.”
Research, however, is where Dr. Oklu sees his lab distinguishing itself from the other sites. His roles as a clinician investigator and the head of the Laboratory of Patient-Inspired Engineering overlap with his work with 3D printing. Among the many advancements he is exploring are about a dozen biomaterials that he hopes can stop bleeding, deliver targeted therapies to tumors, embolize blood vessels and more.
“We’re trying to use our materials to treat aneurysms. The hardest part is making a model,” he says. “We’re thinking maybe we can 3D print the aneurysm to tell us that our biomaterial is working.”
Dr. Oklu sees mostly incremental changes on the horizon in additive manufacturing. “The materials are going to change, the printers are going to change — they’re going to become faster, more widely available, maybe even cheaper — but it will still be the same 3D-printed models.”
Biomaterial printing, though, will be the next revolution in 3D printing, he adds, and he hopes the research he is doing in printing aneurysms will help spur that advancement.
“Continued investment will ensure 3D printing remains an important part of patient-focused care at Mayo Clinic,” Dr. Oklu says. “We’ve come a long way, but we’re just getting started.”

Where it’s going: Florida
In Florida, the group just debuted its newly expanded space. When the program started, they just had a printer on a table, but quickly grew into a space of about 500 square feet where the lab has operated for the last five years. With their new space of about 1,000 square feet, they also added an engineer and biomedical technician dedicated to keeping the printers running.
Dr. Pooley says he recognized there would be a demand for these services in Florida about six years ago and got approval to start a program from J. Mark McKinney, M.D., chair of Florida Department of Radiology at the time.
One of their first patient cases, requested by Si Pham, M.D., now the chair of Cardiothoracic Surgery in Florida, was a cardiac case. “The patient had a tumor in between the left and the right atria,” Dr. Pooley says. “We worked with the radiologist, Dr. Carlos Rojas, and Dr. Pham to segment the model. And we were able to print it on our 3D printer, which had a small build volume — about 6 inches by 6 inches by 6 inches. And the printer prints in just a single material and a single color.”
The result, in white, was printed with about 10 different parts that could be assembled with magnets. The team painted all the parts in different colors — red and blue with the tumor in yellow.
In the early days, Dr. Pooley and whichever staff were working with him on a project would use the same computer-aided design software as was used in Rochester and Arizona. And for projects that exceeded their printing capabilities, they would send the files to Rochester for printing. The models would then be shipped to Florida.
“Rochester was a huge resource that we could learn from,” he says.
Although surgeons could request 3D-printed models from the 3D Anatomic Modeling Unit in Rochester, there is an immense benefit to being able to work with colleagues on the same campus, Dr. Pooley says.
“Over the last six years, we demonstrated our value of being able to print locally in Florida,” Dr. Pooley says. “And part of the value is being able to work closely with surgeons and physicians in Florida.”
Dr. Johnson says her position came with a lot of questions, partly because 3D printing was new to her in general and partly because the medical director role was new in Florida. Her main roles are working with Carleigh Eagle, an engineer with the 3D Anatomic Modeling Unit, and helping with segmentation, as well as evangelizing about 3D printing and the ways it can support the work of other specialists.
“It was a big learning curve. I really didn’t know that much about 3D printing at all, not just the technology and how it worked, but what the applications were in the medical field,” she says, adding that the experience has been eye-opening and rewarding.
Demand for the program’s services, though, was growing, and Dr. Pooley knew it was time to request more space. The expansion of the campus at Mayo Clinic in Florida provided the opportunity.
The value of 3D printing extends beyond clinical care to education and research, Dr. Johnson says. “On the research side, we are active with a lot of different departments and divisions around the hospital, as well as working with the Innovation Exchange and the Simulation Center and helping with educational projects for patients and surgical residents and fellows.”
Dr. Johnson says the Florida team was inspired by a recent visit to Rochester, where they were able to explore the space and learn more about the practice. This further opened their eyes to the possibilities of their growing practice, she says.
“I just feel so fortunate to work for an institution that values and believes in what 3D printing can do for our patients in the present and in the future,” she adds.
With the arrival of Jeffrey Janus, M.D., otorhinolaryngologist, to Mayo Clinic in Florida from Rochester, the need for more resources became more apparent. “He had worked in Rochester with the Anatomic Modeling Unit here to make cutting guides,” Dr. Pooley says. “So when Dr. Janus came to Florida, he brought cutting guides with him. And because we did not have an engineer, when he would put in a request, the engineers in Rochester would create the design for the cutting guides and send the print files to Florida, and we could print them locally.”
The construction boom meant his team would have dedicated space for more printers and people, specifically a full-time engineer dedicated to the 3D Anatomic Modeling Unit. “We were able to add printers, including a new, large-format, multicolor, multimaterial printer, and we were able to hire our first dedicated, full-time engineer,” Dr. Pooley says.
There was broad support for expansion in space and people, Dr. Pooley says, and the stars aligned for the team to hire Eagle, an engineer who was an intern with the 3D Anatomic Modeling Unit in Florida in summer 2021, and Mark P. Lopez, a healthcare biomedical technician, as well as to build a new space in the Campus Support Center, about a half-mile from the clinic buildings.
“With that space we were able to design a facility that met all of our needs,” he says.
Eagle says the group’s transformation in the year since her internship ended is stark.
“Starting out it was like a garage-shop operation,” she says. “You know, we had these specialized cases, and it was all word-of-mouth if you knew that we were there.”
Coming back now as a full-time engineer, it was an emotional moment seeing the new space.
“This was everything we ever could have wanted,” she says. “It feels like the sky’s the limit. It feels like when physicians or researchers or whoever it is come to us and they have a problem, or they have a need, we can figure out a solution.
“And tying back to the leadership, everybody has been like, ‘Yes, make this happen’ for us in Florida. It’s just been so exciting. It’s been a journey.”
And the early returns are promising.
Dr. Pooley says a surgeon recently learned about the 3D Anatomic Modeling Unit — on a Wednesday — and reached out for help with a case. The team quickly turned around a model, which he delivered to the surgeon Sunday.
“The surgeon just glowed, and his eyes brightened up as he held the model in his hands,” Dr. Pooley says. “And as he turned the life-size model around, he said, ‘You know, I need to do this and this in the surgery.’ It was very positive feedback.”
The big picture
Interconnected 3D Anatomic Modeling Units in Arizona, Florida and Rochester allow for cross-site collaborations, and bring different perspectives and experiences to patient care.
“We have very unique minds and are looking for ways to approach and solve different problems, and you’re able to have different, diverse perspectives,” Sears says. “I think all of us joining as a whole, we’re going to be able to solve many complex problems coming up, and we’re going to be able to be more innovative because you’re adding more unique minds to our problem-solving.”
Related articles
[ad_2]
Source link