[ad_1]
Over the past few decades, evidence has been mounting that the average human body temperature is not really 98.6 degrees Fahrenheit. Instead, most people’s baseline is a little bit cooler.
The standard of 98.6 was established over 150 years ago by the German physician Dr. Carl Wunderlich, who reportedly took over a million measurements from 25,000 people. Temperatures ranged from 97.2 to 99.5, and the average was 98.6. Dr. Wunderlich also established 100.4 degrees as “probably febrile.”
However, a study published in September that evaluated the temperatures of more than 126,000 people between 2008 and 2017 found that the average is closer to 97.9 degrees. Other modern-day studies have reported similar numbers.
Experts who study body temperature have differing opinions about why we appear to have gotten cooler over time, and whether that matters when it comes to evaluating fevers and diagnosing infections.
Why 98.6 is off base
Some researchers say it could just be a measurement issue — Dr. Wunderlich might have assessed temperatures using different methods and standards than we do today. One account reports that he used a foot-long thermometer that went into a person’s armpit.
Many factors can influence a body temperature reading, the most significant being where you take it: Rectal temperatures are reliably higher than oral temperatures, which are reliably higher than readings taken from the skin. Body temperature is also influenced by the time of day, whether it’s hot or cold outside and even whether the person just had something to eat or drink. Readings can also vary from thermometer to thermometer, depending on how they are calibrated.
Comparing historical and modern-day data gives you “a hodgepodge mixture of observations,” said Dr. Philip Mackowiak, an emeritus professor of medicine at the University of Maryland School of Medicine, who, in a 1992 paper, was one of the first researchers to scrutinize Dr. Wunderlich’s conclusions. The drop in temperature may be “a true phenomenon,” he added, “but there’s no way of knowing because the data are so varied.”
Other experts think humans really have gotten cooler over the past 150 years. Our temperatures may have declined because “we are so lucky to be healthier than we used to be,” said Dr. Julie Parsonnet, a professor of medicine and of epidemiology and population health at Stanford Medicine, who led the September study on body temperature.
For instance, it could be that many people in Dr. Wunderlich’s sample had slightly elevated temperatures from low-grade inflammation. Better treatment of infections, improved dental care and the development and use of medications like statins and nonsteroidal anti-inflammatory drugs may all have contributed to a decline in inflammation since the 19th century, which in turn lowered people’s average temperature, Dr. Parsonnet said.
Regardless of the reason for the shift, the experts interviewed for this article agreed that 98.6 degrees should no longer be considered the universal human standard. But instead of shifting the average temperature down a degree or so, it should be given as a range, said Dr. Waleed Javaid, a professor of medicine at the Icahn School of Medicine at Mount Sinai, who published a 2019 review paper on body temperature.
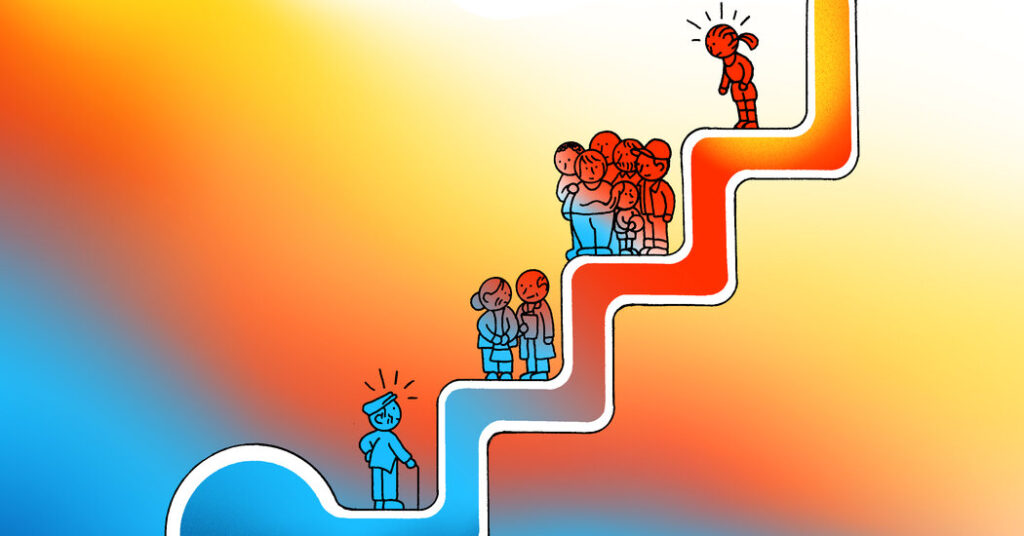
A range would account for the natural variability in temperature that occurs across gender and age — women tend to run slightly warmer than men, and older adults run cooler than younger people. Additionally, everyone’s body temperature fluctuates throughout the day — it is typically lowest in the morning and highest in the late afternoon.
“Like there’s a range for heart rate, there’s a range for blood pressure,” temperature also has a range, Dr. Javaid said.
What counts as a fever
If we redefine “normal” human body temperature, then what registers as abnormal?
The Centers for Disease Control and Prevention says that temperatures of 100.4 and above qualify as a fever — a roughly two-degree increase from 98.6. But if the average human temperature is lower, it’s possible that the temperature indicating a fever could be lower, as well.
Dr. Parsonnet would like to see a personalized approach to fever, where doctors compare each patient against their own baseline so that low-grade fevers aren’t missed in people who run cooler. The mission is somewhat personal for her: Dr. Parsonnet’s mother-in-law has a heart infection that went undiagnosed for months because she never registered as being feverish. Her temperature was around 98.6, but, Dr. Parsonnet said, that “was not normal for her, for her age.”
To Dr. Mackowiak, this individualized approach would be ideal, but it’s unrealistic given the time constraints doctors and nurses are already under.
He and Dr. Javaid are also not as concerned about the possibility of low-grade fevers being missed because of the current temperature standards. Instead of changing the definition of a fever, they said the solution may be to place less of an emphasis on fever overall, and to think of it as one sign among many — something that many doctors already do. (This advice applies to parents, as well as physicians.)
If a temperature is sky-high, that’s important information, Dr. Javaid said, but “the temperature is not the only thing one should look at.”
[ad_2]
Source link